Bronchiectasis
Introduction
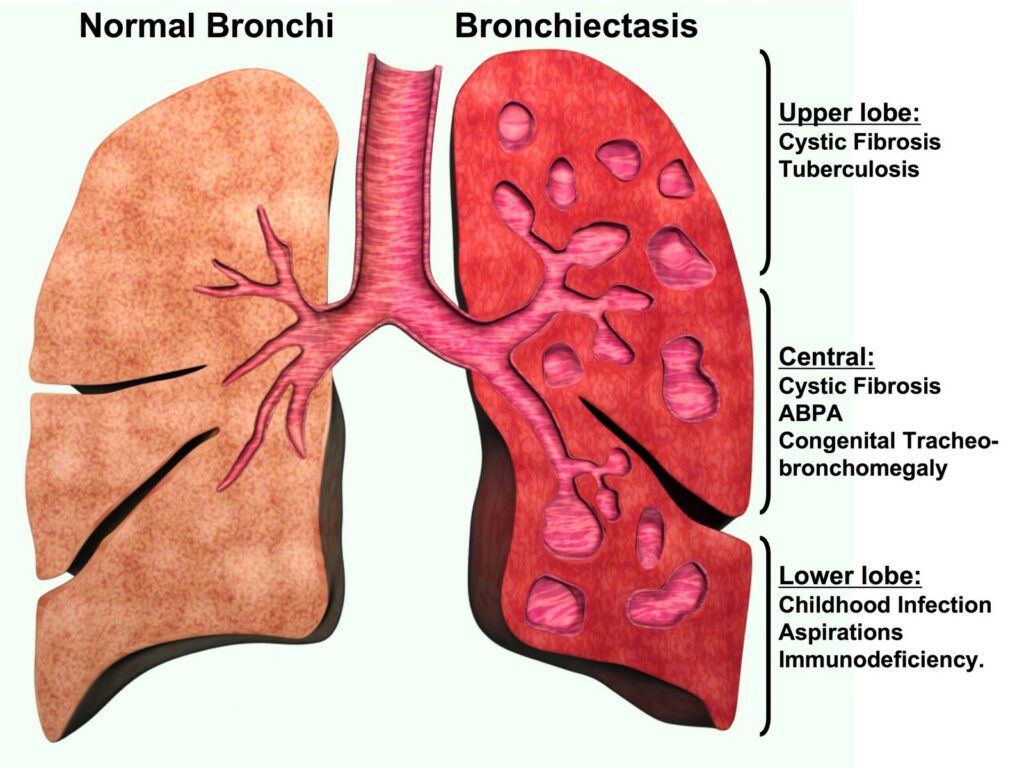
Bronchiectasis is a chronic respiratory condition characterized by abnormal and permanent dilation (widening) of the bronchial tubes (airways) in the lungs. This dilation is typically caused by damage or destruction of the bronchial walls, leading to the accumulation of mucus and bacteria, which can further damage the airways and perpetuate the condition.
Causes
- Severe or recurrent lung infections: Bronchiectasis can develop as a result of severe or recurrent respiratory infections, such as pneumonia, tuberculosis, or whooping cough, which can cause damage to the bronchial walls.
- Cystic fibrosis: Cystic fibrosis, a genetic disorder that affects the lungs and other organs, is a common cause of bronchiectasis in children and young adults.
- Primary ciliary dyskinesia: This inherited condition affects the normal movement of cilia (tiny hair-like structures) in the respiratory tract, leading to impaired mucus clearance and increased susceptibility to infections and bronchiectasis.
- Immunodeficiency disorders: Conditions that weaken the immune system, such as HIV/AIDS, can increase the risk of bronchiectasis due to recurrent or severe lung infections.
- Autoimmune disorders: Rheumatoid arthritis and other autoimmune diseases can lead to inflammation and damage of the bronchial tubes, resulting in bronchiectasis.
- Obstructive lung diseases: Chronic obstructive pulmonary disease (COPD) and severe asthma can, in some cases, contribute to the development of bronchiectasis.
- Aspiration: Recurrent aspiration (inhalation) of stomach contents, foreign objects, or other materials can cause bronchial inflammation and lead to bronchiectasis.
Risk Factors
- Age: Bronchiectasis can occur at any age but is more common in older adults.
- Smoking: Cigarette smoking can damage the lungs and increase the risk of bronchiectasis.
- Environmental exposures: Exposure to air pollution, industrial fumes, or other airborne irritants can contribute to lung damage and bronchiectasis.
- Weakened immune system: Individuals with compromised immune systems due to conditions like HIV/AIDS, cancer, or immunosuppressive medications are at higher risk.
- Childhood respiratory illnesses: Severe respiratory infections during childhood, such as pneumonia or whooping cough, can increase the risk of developing bronchiectasis later in life.
Symptoms
- Persistent cough: A chronic, productive cough that brings up mucus or sputum is one of the most common symptoms of bronchiectasis.
- Wheezing and shortness of breath: The damage to the bronchial tubes can cause wheezing and difficulty breathing, especially during physical activity or exercise.
- Fatigue: The constant coughing and increased work of breathing can lead to fatigue and tiredness.
- Recurrent respiratory infections: Individuals with bronchiectasis are more prone to recurrent lung infections, such as bronchitis or pneumonia.
- Coughing up blood (hemoptysis): In some cases, bronchiectasis can cause coughing up of blood or blood-tinged sputum.
- Clubbing of fingers: A common sign of chronic lung disease, clubbing refers to the enlargement and rounding of the fingertips.
Complications
- Respiratory failure: Severe and untreated bronchiectasis can lead to respiratory failure, a life-threatening condition where the lungs cannot adequately exchange oxygen and carbon dioxide.
- Atelectasis: The accumulation of mucus in the bronchial tubes can cause atelectasis, a condition where the lung or a portion of the lung collapses or does not inflate properly.
- Heart complications: Bronchiectasis can put strain on the heart, increasing the risk of conditions like cor pulmonale (right-sided heart failure) and pulmonary hypertension.
- Hemoptysis: Coughing up significant amounts of blood can occur in severe cases of bronchiectasis, potentially leading to anemia or other complications.
- Reduced quality of life: The persistent cough, breathlessness, and fatigue associated with bronchiectasis can significantly impact an individual’s quality of life.
Differential Diagnosis
- Chronic bronchitis: While chronic bronchitis can cause a persistent cough and mucus production, it does not involve permanent dilation of the bronchial tubes.
- Cystic fibrosis: Cystic fibrosis is a genetic disorder that often leads to bronchiectasis, but it has additional symptoms and complications affecting other organs.
- Tuberculosis: Tuberculosis can cause chronic respiratory symptoms similar to bronchiectasis, but it is an infectious disease caused by a specific bacterium.
- Lung cancer: In some cases, the persistent cough and hemoptysis associated with bronchiectasis may resemble symptoms of lung cancer, which should be ruled out.
- Asthma: While asthma can cause wheezing and shortness of breath, it does not typically involve permanent bronchial dilation or the production of significant amounts of mucus.
Preventions
While bronchiectasis cannot always be prevented, certain measures can reduce the risk or slow the progression of the condition:
- Prompt treatment of respiratory infections: Seeking prompt medical attention and appropriate treatment for respiratory infections can help prevent bronchial damage and the development of bronchiectasis.
- Smoking cessation: Quitting smoking and avoiding exposure to secondhand smoke can help preserve lung health and reduce the risk of bronchiectasis.
- Vaccination: Receiving recommended vaccinations, such as the influenza and pneumococcal vaccines, can help prevent respiratory infections that may contribute to bronchiectasis.
- Management of underlying conditions: Proper management of conditions like cystic fibrosis, primary ciliary dyskinesia, and immunodeficiency disorders can help reduce the risk of bronchiectasis.
Diagnosis
- Physical examination: A healthcare provider will listen to the lungs with a stethoscope and assess for any abnormal breathing sounds or other signs of respiratory disease.
- Chest X-ray: A chest X-ray can reveal abnormalities in the lungs, such as areas of scarring or dilation of the bronchial tubes.
- CT scan: A high-resolution computed tomography (CT) scan is often the preferred imaging test for diagnosing bronchiectasis, as it provides detailed images of the bronchial tubes and lung structures.
- Sputum analysis: An examination of sputum (mucus) samples under a microscope can help identify any bacteria or other organisms present in the lungs.
- Pulmonary function tests: These tests, such as spirometry, measure lung function and can help assess the severity of bronchiectasis.
- Bronchoscopy: In some cases, a bronchoscopy (a procedure that involves inserting a small camera into the bronchial tubes) may be performed to visualize the airways and collect samples for analysis.
Treatments
- Airway clearance techniques: Various techniques, such as chest physiotherapy, positive expiratory pressure (PEP) devices, and flutter valves, can help loosen and clear mucus from the bronchial tubes.
- Medications: Bronchodilators (to relax and open the airways), mucolytics (to thin out mucus), and inhaled or oral antibiotics may be prescribed to manage symptoms and prevent or treat infections.
- Pulmonary rehabilitation: A comprehensive program that includes exercise training, education, and nutritional counseling can improve lung function and overall quality of life for individuals with bronchiectasis.
- Surgery: In severe cases, surgical removal of damaged or dilated bronchial tubes (a procedure called a lobectomy or pneumonectomy) may be considered as a last resort.
- Oxygen therapy: Supplemental oxygen may be necessary for individuals with severe bronchiectasis and low blood oxygen levels.
- Treatment of underlying conditions: Addressing and managing any underlying conditions, such as cystic fibrosis or immunodeficiency disorders, is crucial for the overall management of bronchiectasis.
Important Key Points
- Bronchiectasis is a chronic lung condition characterized by abnormal, permanent widening of the bronchial tubes.
- It is caused by damage or destruction of the bronchial walls, often due to severe infections, cystic fibrosis, or immune system issues.
- Risk factors include age, smoking, environmental exposures, weakened immunity, and childhood respiratory illnesses.
- Key symptoms are persistent cough with mucus production, wheezing, shortness of breath, fatigue, and potential coughing up blood.
- Complications can include respiratory failure, lung collapse, heart problems, and reduced quality of life.
- Differential diagnosis rules out conditions like chronic bronchitis, cystic fibrosis, tuberculosis, lung cancer, and asthma.
- Prevention involves prompt treatment of infections, smoking cessation, vaccinations, and managing underlying conditions.
- Diagnosis uses chest imaging (X-rays, CT scans), sputum analysis, pulmonary function tests, and sometimes bronchoscopy.
- Treatment involves airway clearance techniques, bronchodilators, antibiotics, pulmonary rehab, oxygen therapy, and sometimes surgery.
- Managing any underlying conditions like cystic fibrosis or immunodeficiencies is crucial.
Note: This is a general overview, and it’s always best to consult with a healthcare professional for personalized medical advice and treatment.
When to See a Doctor ?
- See a doctor if you have a persistent cough that lasts for more than a few weeks, especially if you are coughing up large amounts of mucus or phlegm on a regular basis.
- Seek medical attention if you experience recurrent respiratory infections like bronchitis or pneumonia, as these can be signs of an underlying lung condition like bronchiectasis.
- Make an appointment if you notice you are coughing up blood or blood-tinged mucus, as this can be a symptom of bronchiectasis.
- See a doctor if you experience shortness of breath, wheezing, or fatigue during routine activities, as bronchiectasis can cause breathing issues.
- If you have a chronic lung condition like cystic fibrosis, COPD, or a history of childhood respiratory illnesses, report any new or worsening respiratory symptoms to your doctor promptly.
- Seek evaluation if you develop clubbing (enlargement and rounding) of your fingertips or toenails, which can be associated with bronchiectasis and other lung diseases.
- Those with weakened immune systems from HIV, cancer treatment, or autoimmune disorders should report any persistent cough or breathing changes to their doctor.
