Sinusitis
Introduction
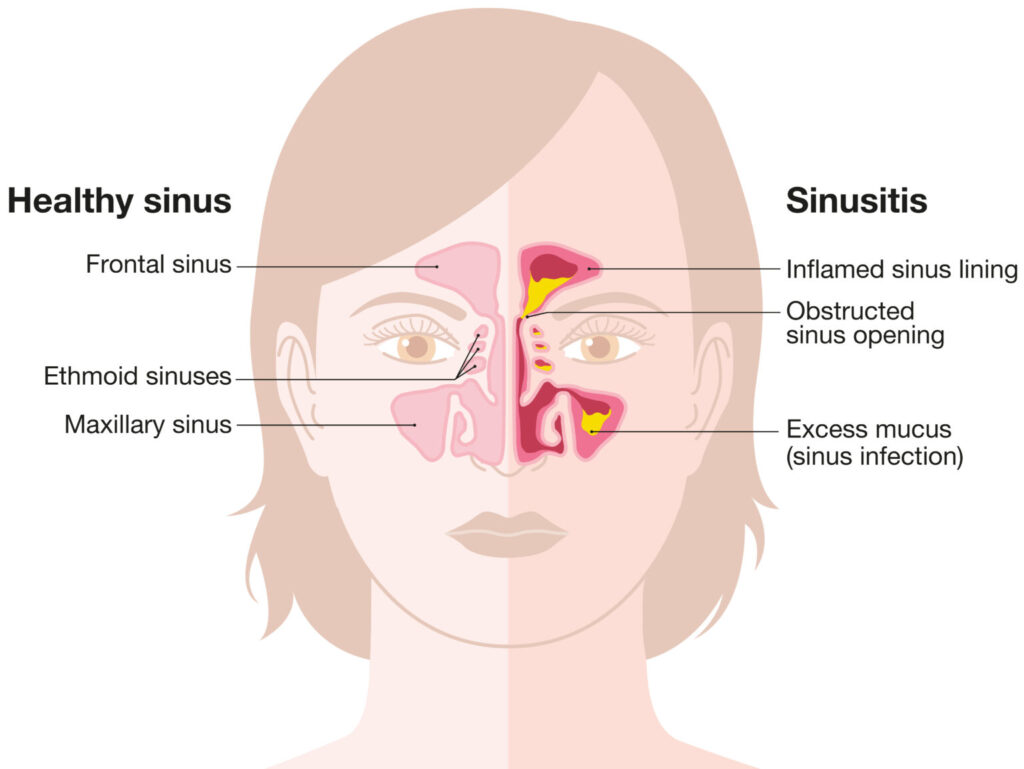
Sinusitis is an inflammation or infection of the sinus cavities, which are air-filled spaces within the bones of the skull. The sinuses are connected to the nasal passages, and their primary function is to produce mucus, which helps trap dust, germs, and other particles before they enter the lungs. When the sinuses become inflamed or blocked, mucus cannot drain properly, leading to sinus pressure, pain, and other symptoms appears.
Causes
- Viral infections: The most common cause of acute sinusitis is a viral infection, such as the common cold or influenza.
- Bacterial infections: Acute sinusitis can sometimes develop from a viral infection and become complicated by a secondary bacterial infection.
- Allergies: Allergic reactions to pollens, dust mites, molds, or other allergens can trigger inflammation in the sinuses, leading to sinusitis.
- Structural abnormalities: Deviated nasal septum, nasal polyps, or other structural abnormalities in the nasal passages can obstruct sinus drainage and increase the risk of sinusitis.
- Environmental factors: Exposure to irritants like cigarette smoke, pollutants, or dry air can irritate the sinus linings and contribute to sinusitis.
Risk Factors
- History of allergies or asthma: Individuals with underlying allergies or asthma are more prone to developing sinusitis.
- Weakened immune system: People with compromised immune systems due to conditions like HIV/AIDS, cancer treatment, or autoimmune disorders are at higher risk of sinusitis.
- Structural abnormalities: Deviated nasal septum, nasal polyps, or other structural abnormalities in the nasal passages can obstruct sinus drainage and increase the risk of sinusitis.
- Environmental exposures: Exposure to irritants like cigarette smoke, pollutants, or dry air can irritate the sinus linings and contribute to sinusitis.
- Dental infections: Infections in the upper teeth or gums can sometimes spread to the sinuses and cause sinusitis.
Symptoms
- Facial pain or pressure: Sinusitis can cause pain, pressure, or a dull ache in the areas surrounding the affected sinuses (forehead, cheeks, around the eyes, or behind the nose).
- Nasal congestion or stuffiness: Inflammation and mucus buildup in the sinuses can lead to nasal congestion, making it difficult to breathe through the nose.
- Thick, discolored nasal discharge: Sinusitis often causes a thick, yellow or green nasal discharge or postnasal drip.
- Headache: The pressure and inflammation in the sinuses can cause headaches, which may be exacerbated by leaning forward or sudden movements.
- Fever: Acute sinusitis, especially when caused by a bacterial infection, may be accompanied by a fever.
- Fatigue and general malaise: Individuals with sinusitis may feel tired and generally unwell.
- Sore throat or cough: Mucus draining from the sinuses can irritate the throat and cause a sore throat or cough.
Complications
- Meningitis: In rare cases, a sinus infection can spread to the membranes surrounding the brain, causing meningitis, a potentially life-threatening condition.
- Orbital cellulitis: If the infection spreads to the eye socket, it can cause orbital cellulitis, which can lead to vision problems or even blindness.
- Osteomyelitis: Untreated sinusitis can sometimes lead to an infection in the bones surrounding the sinuses, known as osteomyelitis.
- Abscess formation: In severe cases, pus can accumulate and form an abscess in the sinus cavities or surrounding areas.
Differential Diagnosis
- Common cold: While a cold can sometimes lead to sinusitis, it typically resolves within a week or two without causing severe sinus symptoms.
- Allergic rhinitis: Allergies can cause nasal congestion and a runny nose, but they typically do not cause facial pain or fever.
- Migraines: Some migraines can cause facial pain and pressure similar to sinusitis, but they are not associated with nasal congestion or discharge.
- Nasal polyps: Nasal polyps can cause nasal obstruction and sinus pressure, but they are typically not accompanied by fever or thick, discolored discharge.
- Dental infections: Infections in the upper teeth or gums can sometimes mimic sinus symptoms and need to be evaluated.
Preventions
- Practice good hygiene: Wash your hands regularly and avoid touching your face to reduce the spread of viruses and bacteria.
- Manage allergies: If you have allergies, take steps to minimize exposure to allergens and manage symptoms with medications or immunotherapy.
- Humidify the air: Dry air can irritate the sinus linings, so using a humidifier can help keep the nasal passages moist and reduce the risk of sinusitis.
- Avoid smoke and pollutants: Exposure to cigarette smoke, chemical fumes, and other pollutants can irritate the sinuses and increase the risk of inflammation.
- Treat underlying conditions: If you have conditions like asthma or structural abnormalities that increase your risk of sinusitis, follow your treatment plan and seek medical advice if symptoms arise.
Diagnosis
- Physical examination: Your healthcare provider will assess your symptoms, examine your face and nasal passages, and may use a light or endoscope to inspect the sinus openings.
- Imaging tests: A CT scan or X-ray may be ordered to visualize the sinus cavities and determine the extent of inflammation or blockage.
- Nasal endoscopy: In some cases, a small camera (endoscope) may be inserted into the nasal passages to examine the sinus openings and identify any structural abnormalities or obstructions.
- Allergy testing: If allergies are suspected as a contributing factor, skin or blood tests may be performed to identify specific allergens.
- Sinus culture: If a bacterial infection is suspected, a sample of nasal discharge or mucus may be collected and cultured to identify the causative organism.
Treatments
The treatment approach for sinusitis depends on the cause, severity, and duration of symptoms.
- Acute Sinusitis Treatment:
– Decongestants and pain relievers: Over-the-counter decongestants and pain relievers like ibuprofen or acetaminophen can help reduce inflammation, relieve sinus pressure, and alleviate pain.
– Saline nasal sprays or rinses: These can help thin out mucus and promote drainage from the sinuses.
– Antibiotics: If a bacterial infection is confirmed or suspected, antibiotics may be prescribed to treat the infection.
– Corticosteroid nasal sprays: These can help reduce inflammation in the nasal passages and sinuses. - Chronic Sinusitis Treatment:
– Nasal corticosteroid sprays: Long-term use of corticosteroid nasal sprays can help manage inflammation and prevent recurrent sinus infections.
– Oral corticosteroids: In severe cases, short courses of oral corticosteroids may be prescribed to reduce inflammation.
– Antibiotics: If a bacterial infection is present, antibiotics may be prescribed to treat the infection.
– Sinus surgery: In cases of structural abnormalities, nasal polyps, or severe, recurrent sinusitis, endoscopic sinus surgery may be recommended to open and drain the sinuses.
– Allergy management: If allergies are a contributing factor, immunotherapy (allergy shots or sublingual drops) or medications like antihistamines or leukotriene inhibitors may be prescribed.
Important Key Points
- Sinusitis is an inflammation or infection of the sinus cavities in the skull.
- Causes include viral infections (most common for acute sinusitis), bacterial infections, allergies, structural abnormalities, and environmental irritants.
- Risk factors are allergies, asthma, weakened immune system, nasal obstructions, and environmental exposures like smoke.
- Key symptoms are facial pain/pressure, nasal congestion, thick discolored discharge, headache, fever, and fatigue.
- Potential complications if untreated include meningitis, vision problems, bone infection, and abscess formation.
- Differential diagnosis rules out conditions like common cold, allergies, migraines, and dental infections.
- Prevention involves good hygiene, allergy management, humidification, and avoiding irritants.
- Diagnosis uses physical exam, imaging tests, endoscopy, allergy testing, and sinus cultures.
- Treatment for acute cases uses decongestants, saline rinses, antibiotics, and corticosteroid sprays.
- Chronic cases may need long-term nasal sprays, oral steroids, antibiotics, sinus surgery, and allergy treatment.
Note: This is a general overview, and it’s always best to consult with a healthcare professional for personalized medical advice and treatment.
When to see a Doctor ?
- See a doctor if sinus symptoms persist beyond 10-14 days without improvement. This may indicate an acute sinus infection requiring medical treatment.
- Seek medical care if you have severe symptoms like intense facial pain/pressure, high fever over 102°F (38.9°C), swelling around the eyes, or symptoms that initially improved but then worsened.
- See a doctor right away for any signs of a potential complication like vision changes, severe headache, stiff neck, or confusion, which could signal a spread of infection.
- Make an appointment if you have frequent recurrent sinus infections (4 or more per year) or symptoms lasting longer than 12 weeks, which may indicate chronic sinusitis.
- If you have nasal polyps, a deviated septum, or other structural abnormalities contributing to sinus blockages, see an ENT (ear, nose, throat) specialist.
- Those with underlying conditions like asthma, cystic fibrosis, or immunodeficiency should see their doctor promptly for sinus symptoms to prevent complications.
- Seek medical evaluation if you experience worrisome symptoms like severe headache, eye swelling, altered vision, stiff neck, or neurological issues.
