Bronchitis
Introduction
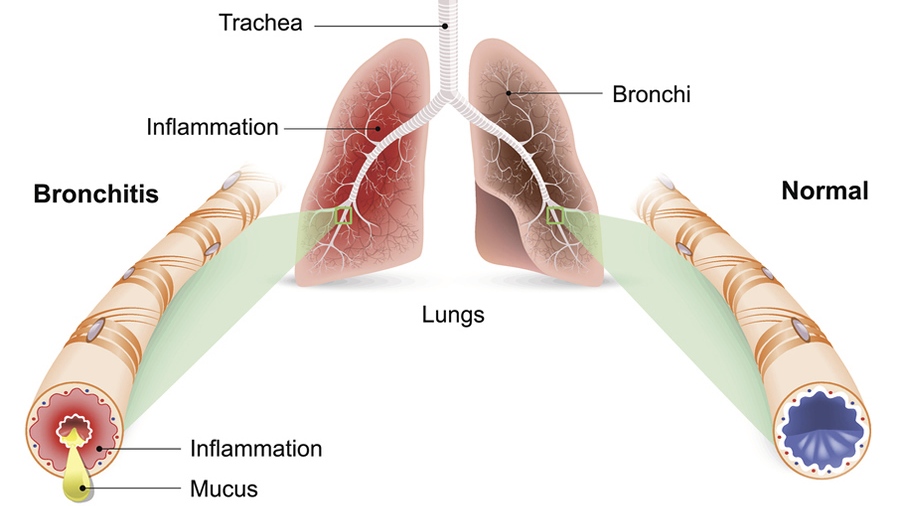
Bronchitis is an inflammatory condition that affects the bronchial tubes, which are the airways that carry air from the trachea (windpipe) into the lungs. It can be classified as acute or chronic, depending on its duration and severity.
Acute bronchitis is a short-term inflammation of the bronchial tubes, typically lasting up to three weeks.
Chronic bronchitis, on the other hand, is a persistent and recurring inflammation that lasts for at least three months out of the year for two consecutive years.
Causes
1. Viral infections: The most common cause of acute bronchitis is a viral infection, usually the same viruses responsible for the common cold or influenza (flu). These viruses can spread through respiratory droplets from coughing or sneezing, or by touching contaminated surfaces and then touching the eyes, nose, or mouth.
2. Bacterial infections: While less common than viral causes, bacterial infections can also lead to bronchitis, particularly if the condition follows a viral illness or if the individual has a weakened immune system. Bacteria such as Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis are known to cause bronchitis.
3. Environmental factors: Exposure to irritants such as cigarette smoke, air pollution, dust, chemical fumes, or other airborne particles can irritate and inflame the bronchial tubes, leading to bronchitis. Chronic exposure to these irritants is a significant risk factor for developing chronic bronchitis.
Risk Factors
1. Smoking: Cigarette smoking is a significant risk factor for developing both acute and chronic bronchitis. The chemicals and irritants in cigarette smoke can directly damage the bronchial tubes and impair the natural defense mechanisms of the respiratory system.
2. Weakened immune system: Individuals with compromised immune systems, such as those undergoing cancer treatment, receiving immunosuppressive medications, or living with HIV/AIDS, are at higher risk of developing bronchitis due to their reduced ability to fight off infections and environmental irritants.
3. Existing respiratory conditions: People with underlying respiratory conditions like asthma, chronic obstructive pulmonary disease (COPD), or cystic fibrosis are more susceptible to developing bronchitis, as their airways are already compromised or inflamed.
4. Age: The elderly and young children are more susceptible due to their weaker immune systems and increased vulnerability to respiratory infections.
5. Occupational exposures: Individuals who work in environments with high levels of dust, chemicals, or other airborne irritants are at a higher risk of developing chronic bronchitis.
Symptoms
1. Persistent cough: A cough that produces mucus or phlegm is a hallmark symptom of bronchitis. The cough may be dry and hacking at first but typically becomes productive as the condition progresses.
2. Wheezing or shortness of breath: Inflammation in the bronchial tubes can cause wheezing, a whistling sound when breathing, or shortness of breath due to the narrowing of the airways.
3. Chest discomfort or tightness: It’s can lead to chest pain or a feeling of tightness or pressure in the chest area, especially during coughing episodes.
4. Fatigue: The inflammation, coughing, and difficulty breathing associated with bronchitis can cause tiredness, weakness, and overall fatigue.
5. Fever (in some cases): Acute bronchitis, especially when caused by a viral infection, may be accompanied by a fever, although this is not always present.
6. Sore throat or hoarseness: Some individuals with bronchitis may experience a sore throat or hoarseness due to the irritation and inflammation in the upper respiratory tract.
7. Nasal congestion or runny nose: It can sometimes be accompanied by nasal symptoms, such as congestion or a runny nose, particularly if it is caused by a viral infection that also affects the upper respiratory tract.
Complications
1. Pneumonia: It’s can sometimes lead to pneumonia, a more serious lung infection that affects the alveoli (air sacs) in the lungs. This is more likely to occur in individuals with weakened immune systems or underlying respiratory conditions.
2. Asthma exacerbation: It’s can trigger or worsen asthma symptoms in individuals with asthma, as the inflammation in the bronchial tubes can further constrict the airways and cause difficulty breathing.
3. Chronic bronchitis: Acute bronchitis can sometimes develop into chronic bronchitis, a long-lasting condition characterized by a persistent cough and mucus production lasting for at least three months out of the year for two consecutive years. Chronic bronchitis is often associated with smoking or exposure to environmental irritants.
4. Respiratory failure: In severe cases, especially in individuals with underlying lung diseases or weakened immune systems, bronchitis can lead to respiratory failure, a life-threatening condition where the lungs are unable to provide enough oxygen to the body.
Differential Diagnosis
Bronchitis shares symptoms with other respiratory conditions, and it is important to differentiate it from these conditions to provide appropriate treatment. The differential diagnosis for bronchitis may include:
1. Asthma: Asthma is a chronic inflammatory condition that causes bronchial tube constriction and wheezing. While bronchitis can also cause wheezing, asthma typically has a more intermittent course and may be triggered by specific allergens or irritants.
2. Pneumonia: Pneumonia is an infection that affects the alveoli (air sacs) in the lungs, causing symptoms like fever, chills, and difficulty breathing. While bronchitis affects the bronchial tubes, pneumonia is a more serious condition that requires prompt treatment with antibiotics.
3. Chronic obstructive pulmonary disease (COPD): COPD is a progressive lung disease that includes chronic bronchitis and emphysema. It is characterized by persistent airflow limitation and breathing difficulties. Individuals with COPD may experience frequent exacerbations of bronchitis.
4. Allergies: Allergic reactions, particularly to airborne allergens like pollen or dust mites, can cause respiratory symptoms similar to bronchitis, such as coughing and wheezing.
5. Sinusitis: Sinusitis, an inflammation of the sinuses, can sometimes cause symptoms like coughing, nasal congestion, and sore throat, which may resemble bronchitis.
Preventions
1. Quit smoking and avoid secondhand smoke: Smoking is a major risk factor for both acute and chronic bronchitis. Quitting smoking and avoiding exposure to secondhand smoke can significantly reduce the risk of developing bronchitis and other respiratory issues.
2. Practice good hygiene: Practicing good hygiene habits, such as washing hands frequently and covering coughs and sneezes, can help prevent the spread of respiratory viruses that can lead to bronchitis.
3. Avoid exposure to air pollutants and irritants: Minimizing exposure to air pollutants, dust, chemical fumes, and other airborne irritants can help prevent bronchial tube inflammation and reduce the risk of bronchitis.
4. Get regular exercise and maintain a healthy lifestyle: Regular physical activity and a balanced diet can help strengthen the immune system and improve overall respiratory health, making it easier for the body to fight off respiratory infections.
5. Consider getting vaccinated: Getting vaccinated against influenza and pneumonia can help prevent respiratory infections that can lead to bronchitis or other complications.
6. Use air purifiers and humidifiers: Installing air purifiers and maintaining proper humidity levels in indoor environments can help reduce exposure to airborne irritants and maintain healthy bronchial tubes.
Diagnosis
Diagnosis of bronchitis typically involves a combination of the following:
1. Medical history and physical examination: The healthcare provider will take a detailed medical history, including symptoms, duration, and potential exposure to irritants or infections. They will also perform a physical examination, listening to the patient’s breathing and checking for wheezing or other abnormal lung sounds.
2. Chest X-ray: A chest X-ray may be ordered to rule out pneumonia or other lung conditions that could be causing the symptoms. It can also help identify any underlying structural abnormalities or complications.
3. Lung function tests (spirometry): Spirometry is a test that measures how much air a person can inhale and exhale, as well as how quickly they can exhale. This test can help assess the severity of bronchitis and determine if there is any airway obstruction or lung function impairment.
4. Sputum analysis: In some cases, a sample of the patient’s sputum (mucus coughed up from the lungs) may be collected and analyzed for the presence of bacteria, viruses, or other pathogens that could be causing the bronchitis.
5. Blood tests: Blood tests may be ordered to check for signs of infection, such as elevated white blood cell count, or to rule out other underlying conditions that could be causing respiratory symptoms.
6. Bronchoscopy: In rare cases, a bronchoscopy (a procedure where a flexible tube with a camera is inserted into the bronchial tubes) may be performed to directly visualize the airways and collect samples for further analysis.
Treatments
The treatment approach for bronchitis depends on whether it is acute or chronic, as well as the underlying cause and severity of the condition.
- Acute Bronchitis Treatment:
– Rest: Getting plenty of rest can help the body recover from acute bronchitis.
– Increased fluid intake: Drinking plenty of fluids helps thin out mucus and makes it easier to cough up.
– Over-the-counter cough suppressants or expectorants: Cough suppressants can help control dry, hacking coughs, while expectorants can help loosen and expel mucus.
– Bronchodilators: If wheezing is present, bronchodilators (inhaled medications that relax and open the airways) may be prescribed.
– Antibiotics: Antibiotics are generally not recommended for acute bronchitis caused by a viral infection, as they are ineffective against viruses. However, if a bacterial infection is suspected or confirmed, antibiotics may be prescribed.
- Chronic Bronchitis Treatment:
– Bronchodilators: Inhaled bronchodilators, such as albuterol or ipratropium, can help relax and open the airways, making it easier to breathe.
– Corticosteroids: Inhaled or oral corticosteroids may be prescribed to reduce inflammation in the bronchial tubes.
– Oxygen therapy: In severe cases or during acute exacerbations, supplemental oxygen may be necessary to improve oxygen levels in the blood.
– Pulmonary rehabilitation: This comprehensive program, which includes exercise training, education, and nutritional counseling, can help manage symptoms and improve quality of life for individuals with chronic bronchitis or COPD.
– Smoking cessation: Quitting smoking is crucial for managing and preventing further progression of chronic bronchitis and other respiratory conditions.
Important Key Points
- Bronchitis is an inflammation of the bronchial tubes (airways) in the lungs, classified as acute (short-term) or chronic (long-lasting).
- Common causes include viral infections, bacterial infections, and environmental irritants like cigarette smoke, air pollution, and chemical fumes.
- Risk factors include smoking, weakened immune system, existing respiratory conditions (asthma, COPD, cystic fibrosis), age (elderly and young children), and occupational exposures.
- Symptoms: persistent cough with mucus production, wheezing or shortness of breath, chest discomfort or tightness, fatigue, fever (in some cases), sore throat, nasal congestion.
- Complications: pneumonia, asthma exacerbation, chronic bronchitis, respiratory failure (in severe cases).
- Differential diagnosis includes asthma, pneumonia, COPD, allergies, and sinusitis.
- Prevention involves quitting smoking, practicing good hygiene, avoiding air pollutants and irritants, maintaining a healthy lifestyle, and considering vaccinations.
- Diagnosis involves medical history, physical examination, chest X-ray, lung function tests (spirometry), sputum analysis, and sometimes blood tests or bronchoscopy.
- Treatment options include rest and fluids, over-the-counter medications for symptom relief, antibiotics (if bacterial infection), bronchodilators or inhaled corticosteroids (for underlying respiratory conditions), oxygen therapy (in severe cases), pulmonary rehabilitation (for chronic bronchitis), and hospitalization (in severe cases).
- Lifestyle changes, such as quitting smoking, avoiding irritants, and maintaining a healthy lifestyle, are crucial for managing bronchitis effectively.
Note: This is a general overview, and it’s always best to consult with a healthcare professional for personalized medical advice and treatment.
When to See a Doctor ?
- See a doctor if you have a cough that persists for more than 3 weeks. This could be a sign of chronic bronchitis or another underlying condition.
- Seek medical attention if you experience shortness of breath, wheezing, or difficulty breathing. These can indicate a more severe respiratory issue.
- If you have a high fever (over 101°F or 38.3°C), it’s advisable to see a doctor, as this may signal a secondary infection like pneumonia.
- Consult a doctor if you cough up blood or greenish-yellow phlegm, which can indicate a bacterial infection.
- See a doctor right away if your symptoms are severe, such as chest pain, confusion, or lips/fingernails turning blue, which suggest breathing difficulties.
- Those with underlying conditions like asthma, COPD, heart disease, or weakened immune systems should see a doctor promptly for bronchitis symptoms.
- Seek medical care if symptoms initially improve but then worsen or you develop new symptoms like fever.
- If you are an older adult or have young children with bronchitis symptoms, it’s best to get evaluated due to their higher risk of complications.
The key is not to delay seeking medical care if bronchitis symptoms persist beyond 2-3 weeks, worsen, or become severe. Early treatment is important to prevent potential complications.
