Pneumonia
Introduction
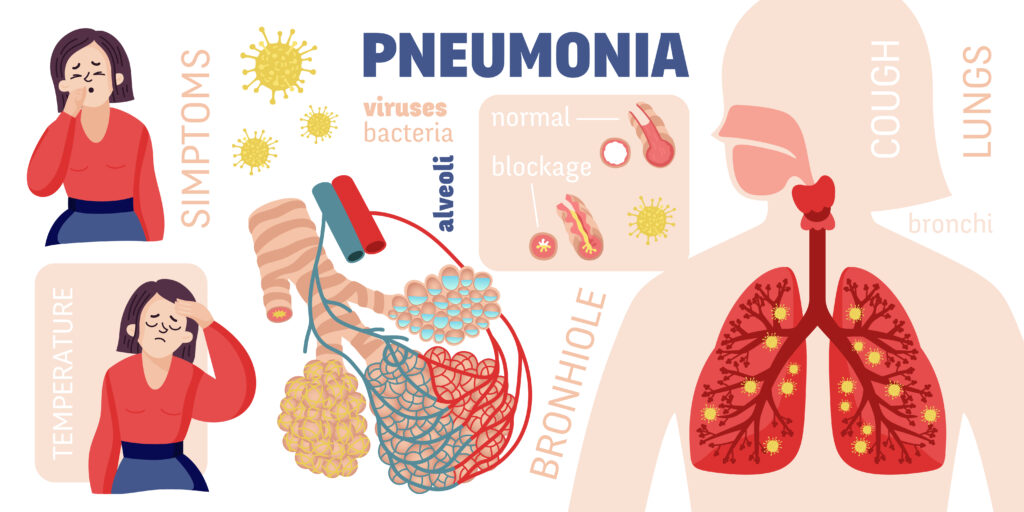
Pneumonia is a serious respiratory infection that affects the lungs, specifically the alveoli (air sacs) responsible for the exchange of oxygen and carbon dioxide. It can be caused by various microorganisms, including viruses, bacteria, and fungi, and can range in severity from mild to life-threatening.
Causes
1. Viral infections: Influenza (flu) viruses, respiratory syncytial virus (RSV), and SARS-CoV-2 (the virus responsible for COVID-19) are common viral causes of pneumonia.
2. Bacterial infections: Streptococcus pneumoniae (the most common bacterial cause), Haemophilus influenzae, Staphylococcus aureus, and Mycoplasma pneumoniae are some of the bacteria that can lead to pneumonia.
3. Fungal infections: It’s can also be caused by fungal pathogens, such as Pneumocystis jirovecii, which is particularly dangerous for individuals with weakened immune systems.
4. Aspiration: Inhaling food, liquid, or vomit into the lungs can lead to a type of pneumonia called aspiration pneumonia.
Risk Factors
1. Age: Infants, young children, and the elderly are at increased risk of developing pneumonia due to their weaker immune systems.
2. Chronic medical conditions: People with chronic illnesses like heart or lung disease, diabetes, cancer, or HIV/AIDS have a higher risk of pneumonia.
3. Weakened immune system: Individuals with compromised immune systems, whether due to medications, cancer treatment, or other conditions, are more susceptible to pneumonia.
4. Smoking: Cigarette smoking damages the lungs and increases the risk of developing respiratory infections, including pneumonia.
5. Recent viral illness: Having a recent viral infection, such as the flu or a common cold, can make an individual more vulnerable to developing bacterial pneumonia.
6. Hospitalization or nursing home residence: Exposure to various pathogens in healthcare settings can increase the risk of pneumonia, especially for those with underlying health conditions.
Symptoms
1. Cough: A persistent cough, often producing phlegm or mucus, is a common symptom of pneumonia.
2. Fever: Most cases of pneumonia are accompanied by a fever, which can range from mild to high.
3. Shortness of breath or rapid breathing: As the lungs become inflamed and filled with fluid, breathing becomes more difficult.
4. Chest pain: It’s can cause a sharp or dull pain in the chest when breathing or coughing.
5. Fatigue and weakness: The body’s effort to fight the infection and the lack of proper oxygenation can lead to feelings of extreme tiredness and weakness.
6. Chills and sweating: Chills, shivering, and sweating are common symptoms of pneumonia, especially when accompanied by a fever.
7. Nausea, vomiting, and diarrhea: These symptoms may occur, particularly in young children with pneumonia.
Complications
1. Respiratory failure: In severe cases, It can lead to respiratory failure, where the lungs are unable to provide enough oxygen to the body.
2. Sepsis: It’s can sometimes cause the infection to spread to the bloodstream, leading to sepsis, a life-threatening condition.
3. Lung abscesses: Pockets of pus or infected fluid can form in the lungs, known as lung abscesses, which may require surgical drainage.
4. Pleural effusion: Fluid can accumulate between the membranes lining the lungs and the chest cavity, causing breathing difficulties.
5. Acute respiratory distress syndrome (ARDS): In severe cases, It can lead to ARDS, a life-threatening condition where the lungs cannot provide enough oxygen to the body.
Differential Diagnosis
Pneumonia shares symptoms with other respiratory conditions, and it is important to differentiate it from these conditions to provide appropriate treatment. The differential diagnosis for pneumonia may include:
1. Bronchitis: Bronchitis is an inflammation of the bronchial tubes, causing a persistent cough and wheezing, but without the fever and chest pain associated with pneumonia.
2. Asthma: Asthma is a chronic respiratory condition characterized by wheezing, shortness of breath, and coughing, but without the presence of fever or lung inflammation.
3. Influenza (flu): The flu is a viral respiratory illness that can cause similar symptoms to pneumonia, but it typically does not cause the severe lung involvement seen in pneumonia.
4. Tuberculosis: Tuberculosis is a bacterial infection that primarily affects the lungs and can mimic some of the symptoms of pneumonia, such as coughing, fever, and shortness of breath.
5. Lung cancer: In some cases, lung cancer can cause symptoms similar to pneumonia, such as coughing, shortness of breath, and chest pain.
Preventions
1. Vaccination: Getting vaccinated against influenza, pneumococcal disease, and other respiratory infections can help prevent pneumonia caused by these pathogens.
2. Proper hand hygiene: Frequent handwashing and avoiding contact with respiratory secretions can reduce the spread of infections that can lead to pneumonia.
3. Smoking cessation: Quitting smoking can significantly reduce the risk of developing pneumonia and other respiratory conditions.
4. Managing underlying conditions: Properly managing chronic medical conditions, such as asthma, COPD, or diabetes, can lower the risk of developing pneumonia.
5. Avoiding exposure: Limiting exposure to individuals with respiratory infections and practicing good respiratory etiquette (covering coughs and sneezes) can help prevent the spread of infections that may cause pneumonia.
Diagnosis
1. Medical history and physical examination: The healthcare provider will take a detailed medical history, including symptoms, recent illnesses, and potential exposures. They will also perform a physical examination, listening to the lungs for abnormal sounds and checking for other signs of respiratory distress.
2. Chest X-ray: A chest X-ray is a standard diagnostic tool for pneumonia, as it can reveal the presence of inflammation or fluid in the lungs.
3. Blood tests: Blood tests may be ordered to check for signs of infection, such as elevated white blood cell count, or to identify the specific pathogen causing the pneumonia.
4. Sputum or mucus sample analysis: A sample of the patient’s sputum or mucus may be collected and analyzed for the presence of bacteria, viruses, or other pathogens.
5. Pulse oximetry: This non-invasive test measures the oxygen saturation level in the blood, which can help assess the severity of pneumonia and the need for supplemental oxygen.
6. CT scan or bronchoscopy: In some cases, a CT scan or bronchoscopy (a procedure where a flexible tube with a camera is inserted into the bronchial tubes) may be performed to obtain more detailed images of the lungs or to collect samples for further analysis.
Treatments
1. Antibiotics: If pneumonia is caused by a bacterial infection, antibiotics will be prescribed to target the specific bacteria responsible. The choice of antibiotic will depend on the type of bacteria and the severity of the infection.
2. Antiviral medications: For pneumonia caused by viral infections, such as influenza or COVID-19, antiviral medications may be prescribed to help alleviate symptoms and reduce the duration of the illness.
3. Oxygen therapy: In cases of severe pneumonia, supplemental oxygen may be provided to ensure adequate oxygenation and prevent respiratory failure.
4. Supportive care: Supportive care measures, such as pain relievers, fever reducers, and fluid intake, can help manage symptoms and support the body’s recovery.
5. Hospitalization: Severe cases of pneumonia may require hospitalization for close monitoring, intravenous antibiotics or antivirals, and respiratory support, if needed.
6. Ventilator support: In cases of respiratory failure, mechanical ventilation may be necessary to assist with breathing until the infection resolves.
7. Adjunctive therapies: In certain cases, additional therapies, such as corticosteroids or immunomodulatory drugs, may be used to help control inflammation or support the immune system’s response.
Important Key Points
- Pneumonia is a serious respiratory infection affecting the lungs, specifically the alveoli (air sacs).
- Causes include viral infections (influenza, RSV, SARS-CoV-2), bacterial infections (Streptococcus pneumoniae, Haemophilus influenzae), and fungal infections.
- Risk factors include age (infants, elderly), chronic medical conditions, weakened immune system, smoking, recent viral illness, and hospitalization/nursing home residence.
- Symptoms: cough, fever, shortness of breath, chest pain, fatigue, chills, sweating, nausea/vomiting.
- Complications: respiratory failure, sepsis, lung abscesses, pleural effusion, acute respiratory distress syndrome (ARDS).
- Differential diagnosis includes bronchitis, asthma, influenza, tuberculosis, lung cancer.
- Prevention involves vaccinations, hand hygiene, smoking cessation, managing underlying conditions, avoiding exposure.
- Diagnosis through medical history, physical examination, chest X-ray, blood tests, sputum analysis, pulse oximetry, CT scans, bronchoscopy.
- Treatment depends on the cause – antibiotics for bacterial, antivirals for viral, oxygen therapy, supportive care, hospitalization, ventilator support.
- Early diagnosis and prompt treatment are crucial to prevent complications and facilitate recovery.
- Vaccination and preventive measures are key to reducing the risk of pneumonia.
Note: This is a general overview, and it’s always best to consult with a healthcare professional for personalized medical advice and treatment.
It’s important to follow the prescribed treatment plan and seek medical attention promptly if symptoms persist or worsen, as pneumonia can progress rapidly and lead to serious complications if left untreated.
